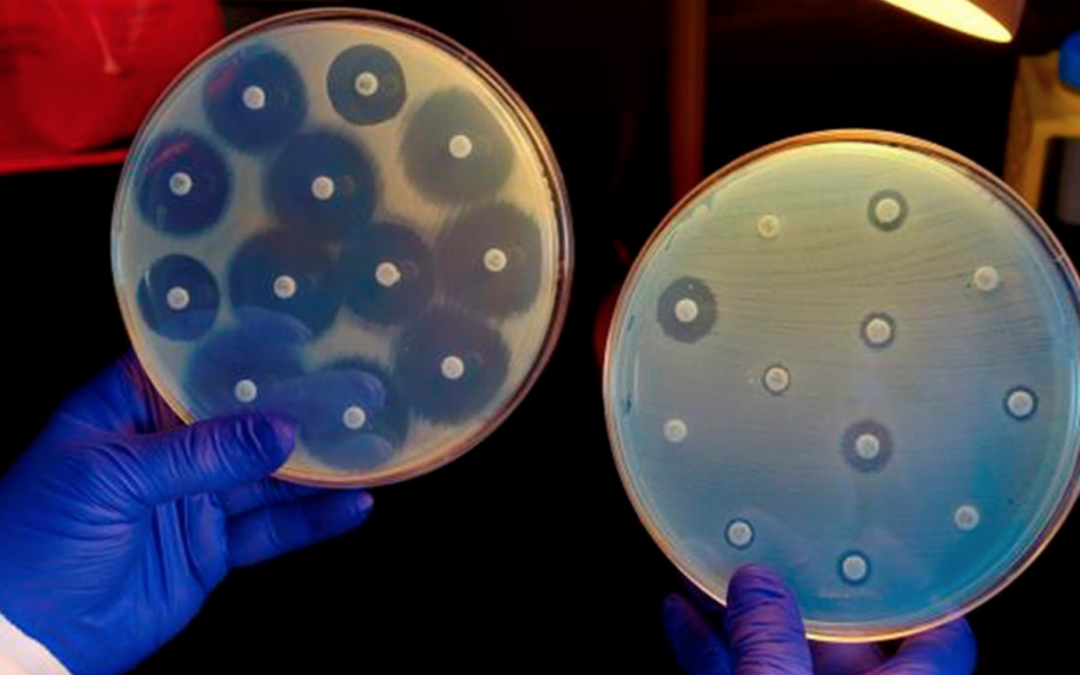
The research, published on Wednesday in the journal Scientific Reports, demonstrates for the first time how bacteria respond to adverse conditions, such as when they are subjected to drug treatments.
The research group on bacterial infections and antimicrobial therapies of the IBEC, led by Dr. Eduard Torrents, has specialized in the study of the bacterial strain ‘Pseudomonas aeruginosa’, which can cause serious chronic pulmonary infections in patients with cystic fibrosis (CF). to those that severely damage lung function, increasing the risk of respiratory failure and even causing death.
As explained by Torrents, one of the global regulatory systems of the ‘Pseudomona aeruginosa’, AlgZR, is responsible for converting bacteria into the phenotype associated with chronic disease, known as mucoid.
By studying the regulation of these bacteria under stressful conditions, the researchers discovered that AlgZR also controls how DNA synthesis is modulated, allowing bacteria to react to these conditions.
“This response could also explain how bacteria react or adapt to other stressful situations, such as being attacked by antibiotics,” Torrents summarized.
“This link between stress and the AlgZR system provides, for the first time, a molecular explanation of how bacteria can continue to divide under antibiotic treatment,” the researcher said.
According to Torrents, “in most bacterial species, there are two component systems similar to AlgZR, so more experiments will be carried out to evaluate if these results are extensible to other bacterial species.”
At the end of 2016, the research line on cystic fibrosis of the Eduard Torrents group received funding from the “La Caixa” Banking Foundation, an impulse that, according to the financing entity, will last for 3 years, and which will be linked to the financing of the Spanish Cystic Fibrosis Foundation.
Source: antena3.com